By: Fabiha Karim
Patient Details: A 32-year-old male presented to our ophthalmologist’s retina clinic with a history of a traumatic injury to his right eye. The patient reported being hit in the right eye with a beer bottle, resulting in immediate visual impairment and pain.
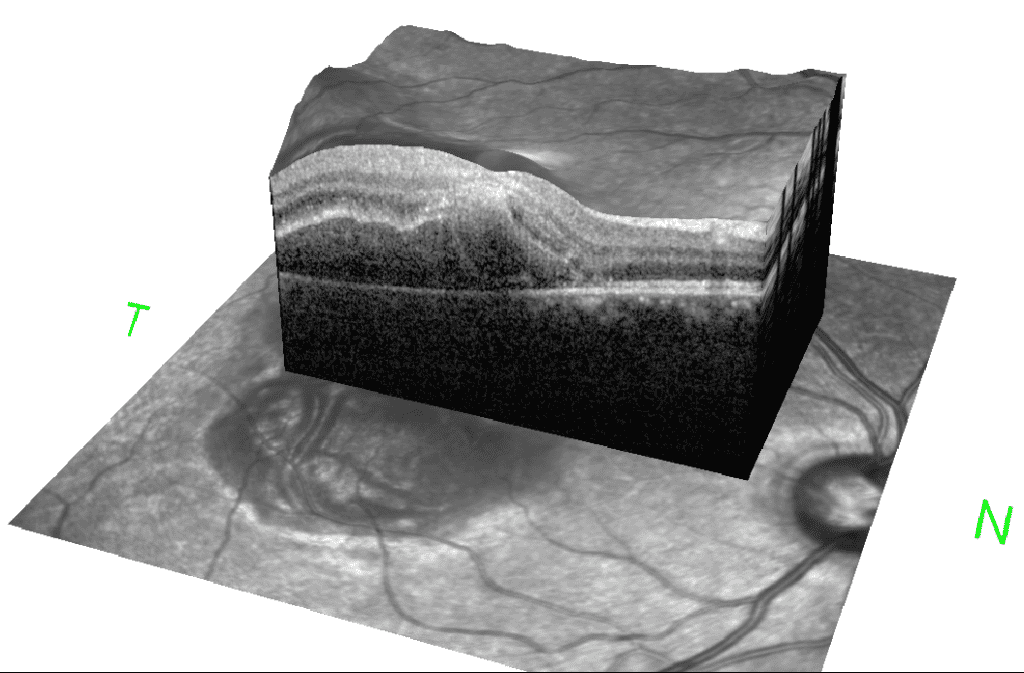
Clinical Presentation: Upon examination, the patient exhibited reduced visual acuity in the right eye, with a visual acuity of Count Finger (CF) at one foot. Slit-lamp biomicroscopy revealed a localized foveo-macular retinal detachment with a subretinal hemorrhage, consistent with a choroidal rupture. Fundus examination confirmed the presence of a choroidal rupture associated with the macular region. No signs of proliferative vitreoretinopathy or other retinal pathologies were noted in the fellow eye.
Treatment Approach: Dr. Shah, a retinal ophthalmologist, was consulted for the management of this challenging case. After a thorough discussion of treatment options and risks, a decision was made to proceed with a pneumatic retinopexy. The procedure involved the injection of 0.3 cc’s of perfluoropropane (C3F8) gas into the vitreous cavity, followed by face-down positioning to promote retinal reattachment.
Outcome: Following the pneumatic retinopexy and adherence to the prescribed face-down positioning regimen, the patient exhibited remarkable improvement in his visual acuity. Serial examinations demonstrated successful reattachment of the fovea, with visual acuity improving from Count Finger at one foot to 20/40. Despite mild perifoveal scarring, the patient’s visual function showed a significant and favorable outcome.
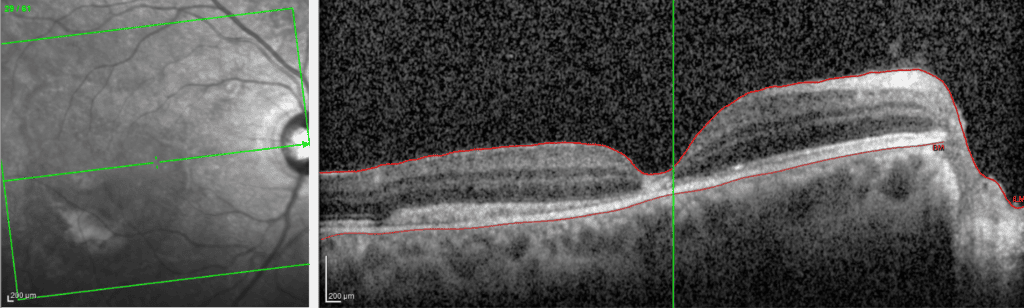
Discussion: Choroidal ruptures are a rare consequence of blunt ocular trauma and can lead to various retinal complications, including retinal detachment. In this case, the localized foveo-macular retinal detachment resulting from a choroidal rupture required a tailored intervention to promote retinal reattachment. Pneumatic retinopexy with the administration of C3F8 gas, combined with face-down positioning, proved to be an effective strategy in achieving successful anatomical and functional outcomes.
It is important to note that despite the successful reattachment, mild perifoveal scarring was observed. While this scarring may contribute to some residual visual impairment, the overall improvement in visual acuity signifies a significant therapeutic success.
Future Considerations: The patient’s clinical course warrants ongoing monitoring, as a new choroidal neovascular membrane has been identified. Given the potential for further visual impairment and complications, the patient may benefit from anti-vascular endothelial growth factor (anti-VEGF) therapy by a retinal ophthalmologist. This targeted treatment approach aims to inhibit neovascularization and preserve visual function in the presence of choroidal neovascularization.
In conclusion, the presented case highlights the successful management of a foveo-macular retinal detachment secondary to a choroidal rupture through pneumatic retinopexy and face-down positioning. The patient’s substantial improvement in visual acuity, despite mild scarring, underscores the importance of tailored therapeutic interventions in cases of traumatic ocular injury involving choroidal breaks. Continued vigilance and appropriate intervention, such as anti-VEGF therapy, will be essential in ensuring optimal visual outcomes for the patient.
Early intervention by a retinal ophthalmologist can rescue vision in even the most severe of issues with the macula, retina, or vitreous. Click here to book an appointment for you or your loved one today.
Question: Great patient, I’m curious was there a schedule for the face down positioning? Was it so many hours per day with a certain time break between positioning ?
Great question Susan! Yes he was face down for 24 hours a day for the first week, then only while sleeping until the gas bubble dissipated 1 month later.