By: Michael Berman, Delaney Plecha, and Chirag Shah MD MPH
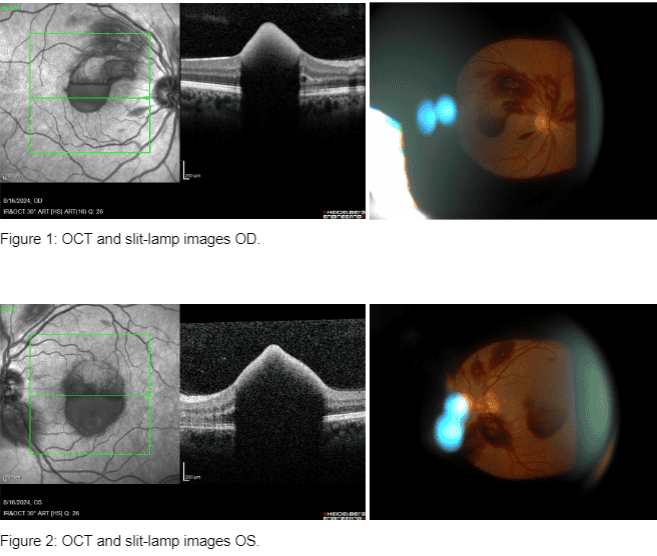
| Introduction A 35-year-old male presented to our clinic with significant near vision loss. The patient, who has a known history of leukemia with treatment such as chemotherapy, had a visual acuity (VA) measured at 20/200 in the right eye (OD) and 20/100 in the left eye (OS). Background Information Thrombocytopenia is defined as a platelet count that falls below the lower limit of normal range: 150,000/mL (for adults). It can be caused by decreased platelet production, increased platelet destruction, or sequestration of platelets in the spleen. In patients with leukemia, thrombocytopenia is frequently a consequence of bone marrow infiltration by malignant cells, chemotherapy, or radiation therapy. Thrombocytopenia increases the risk of bleeding complications, including retinal hemorrhages, which can significantly impact vision. Examination Findings Further examination included Optical Coherence Tomography (OCT) imaging and a detailed retina evaluation, which revealed the following findings in both eyes (OU): vitreous hemorrhage (significant hemorrhage in the vitreous cavity), sub-retinal hemorrhage (hemorrhage located beneath the retinal layers), sub-Internal Limiting Membrane (ILM) hemorrhage (hemorrhage beneath the ILM), foveal involvement (hemorrhages impacting both foveae, contributing to significant visual acuity loss) |
Diagnosis & Follow Up plan
Based on the patient’s history and Dr. Shah’s clinical findings, bloodwork was obtained, and the patient was diagnosed with low platelets (thrombocytopenia)..
Management of this condition involved coordinating with the patient’s hematologist and oncologist for platelet infusions to address thrombocytopenia and prevent further hemorrhagic complications.
Going forward, regular follow-up appointments were recommended in order to continue monitoring hemorrhage resolution and platelet levels.
Discussion
The retinal findings in this patient, including vitreous hemorrhage, sub-retinal hemorrhage, and sub-ILM hemorrhage, are indicative of severe retinal involvement.
The management of such cases requires a
multidisciplinary approach, involving both ophthalmologists and hematologists/oncologists to address the underlying systemic condition.
Platelet infusions are critical in this scenario to prevent further hemorrhagic events and to promote the resolution of existing hemorrhages. Close monitoring of the patient’s platelet counts and retinal status is essential to ensure optimal outcomes. Additionally, the patient’s leukemia treatment plan may need
to be adjusted to manage the thrombocytopenia more effectively.
Conclusion
Our patient’s hemorrhages resolved after his platelets normalized. This case underscores the need for a multidisciplinary approach to manage retinopathies in patients with systemic disorders, emphasizing the importance of early diagnosis and intervention to prevent further vision loss. In this case, it also helped avoid procedures like injections and surgery.
References
1. Tripathy, Koushik, and Bhupendra C. Patel. “Purtscher Retinopathy.” StatPearls [Internet].,
U.S. National Library of Medicine, 25 Aug. 2023, www.ncbi.nlm.nih.gov/books/NBK542167/.
2. Jinna, Sruthi, and Paras B. Khandhar. “Thrombocytopenia.” StatPearls [Internet]., U.S.
National Library of Medicine, 4 July 2023, www.ncbi.nlm.nih.gov/books/NBK542208/