By: Chista Niknam and Chirag Shah MD
Diabetic retinopathy (DR) is a common eye condition that affects people with diabetes, and it is a leading cause of blindness in adults. It occurs when high blood sugar levels damage the blood vessels in the retina, the light-sensitive layer at the back of the eye. The condition progresses in stages, from mild to severe, and can result in vision loss if left untreated.
All treatments are available at our clinic, and Dr. Shah evaluates each patient individually to determine the most appropriate therapy tailored to their unique situation. Click here to Book Online or Refer A Patient for diabetic eye examination and/or treatment.
Diabetic macular edema (DME) is a specific complication of DR that occurs when the damaged blood vessels in the retina leak fluid into the macula (the central part of the retina responsible for sharp, detailed vision). This fluid accumulation causes the macula to swell, leading to blurred or distorted central vision. While DR affects the entire retina, DME is primarily a result of fluid buildup in the macula, often causing more noticeable vision problems like difficulty reading or recognizing faces.
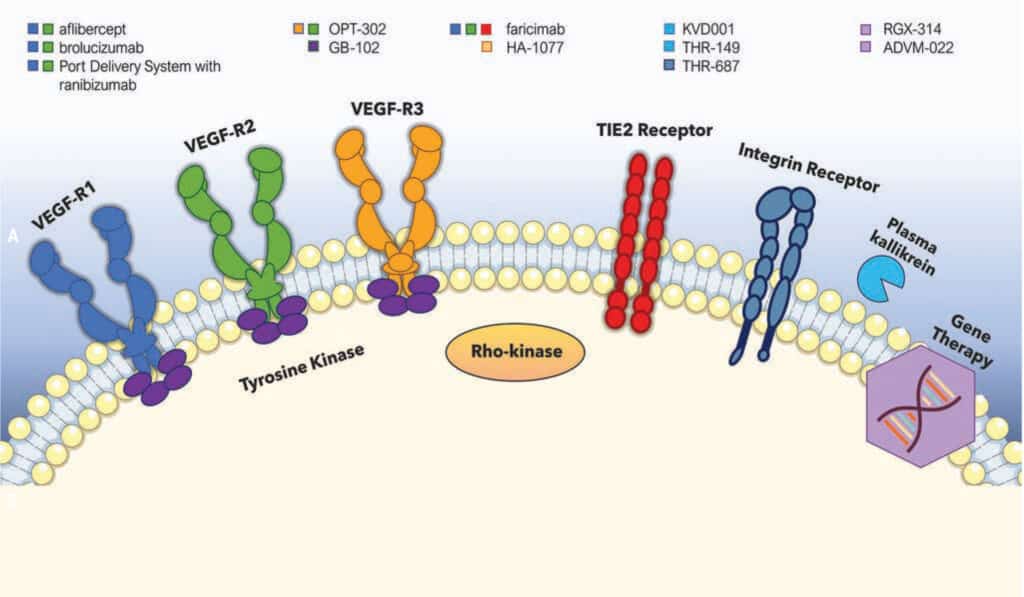
Treatment aims to reduce abnormal blood vessel growth, fluid leakage, and inflammation in the retina, helping to preserve vision. Below are common medical treatments and how they work:
1. Vabysmo (Faricimab)
Mechanism:
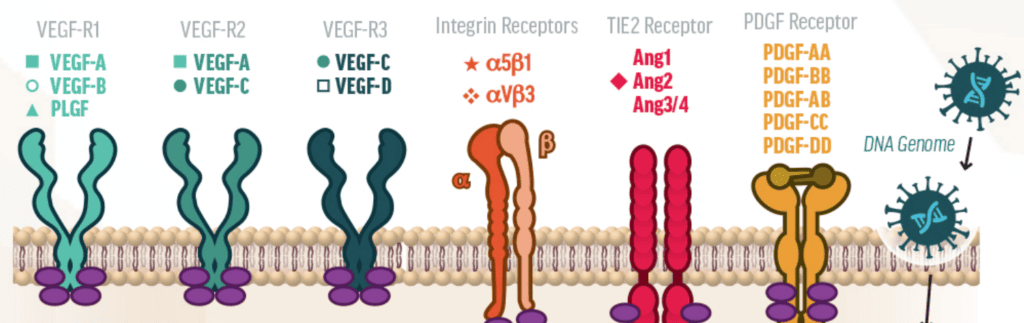
- Vabysmo is a bispecific antibody that targets both VEGF-A (vascular endothelial growth factor) and Angiopoietin-2 (Ang-2), a protein involved in vascular leakage and inflammation. By blocking both, it helps stabilize blood vessels and reduce retinal swelling.
Visual Outcomes:
- Vabysmo has shown significant improvements in visual acuity (sharpness of vision) in clinical trials for both DR and DME. Its dual-target approach (VEGF-A and Ang-2) helps reduce abnormal blood vessel growth and leakage, leading to better vision preservation.
Anatomical Outcomes:
- Vabysmo reduces macular edema and central retinal thickness (CRT), which are common issues in DME. The drug’s dual mechanism provides long-lasting effects, meaning fewer injections are often required to achieve anatomical improvements.
2. Eylea (Aflibercept)
Mechanism:
- Eylea is a recombinant fusion protein that blocks VEGF-A, VEGF-B, and Placental Growth Factor (PlGF). By targeting these factors, Eylea prevents abnormal blood vessel formation and leakage, which reduces swelling and preserves retinal health.
Visual Outcomes:
- Eylea has demonstrated consistent improvements in visual acuity for patients with DME and DR. It is one of the most commonly used treatments due to its ability to stabilize or improve vision over time.
Anatomical Outcomes:
- Eylea reduces macular edema and central retinal thickness (CRT) effectively. Patients experience significant decreases in retinal fluid and improvements in the retina’s structure, helping to stabilize vision.
3. Avastin (Bevacizumab)
Mechanism:
- Avastin is a monoclonal antibody that targets VEGF-A, reducing the growth of abnormal blood vessels and preventing leakage in the retina. By inhibiting VEGF, it reduces vascular permeability and inflammation.
Visual Outcomes:
- While not FDA-approved for ophthalmic use, Avastin is frequently used off-label for improving visual acuity in patients with DR and DME. It has shown significant benefits, though patients may require more frequent injections compared to Eylea or Vabysmo.
Anatomical Outcomes:
- Avastin helps reduce retinal edema and decrease retinal thickness. However, since it is not specifically designed for eye use, it may need to be administered more often to maintain these anatomical improvements.
4. Ozurdex (Dexamethasone Intravitreal Implant)
Mechanism:
- Ozurdex is a biodegradable intravitreal implant that releases dexamethasone, a corticosteroid that reduces inflammation and retinal edema. It works by inhibiting inflammatory mediators that contribute to fluid leakage in the retina.
Visual Outcomes:
- Ozurdex is effective for patients who do not respond well to anti-VEGF treatments. It can lead to improvements in visual acuity by reducing inflammation and swelling. However, it may have a higher risk of side effects like cataracts and increased eye pressure with long-term use.
Anatomical Outcomes:
- Ozurdex is particularly effective at reducing macular edema and improving the anatomical structure of the retina by inhibiting inflammatory cytokines. Its effect tends to last for several months, but the risks associated with steroid use (like increased intraocular pressure) must be considered.
5. Eylea HD (Aflibercept with Hydroxypropylmethylcellulose)
Mechanism:
- Eylea HD is essentially a modified version of Eylea (aflibercept) combined with hydroxypropylmethylcellulose (HPMC). The addition of HPMC increases the viscosity of the drug, helping it remain in the eye longer and extending its therapeutic effect, while still blocking VEGF-A, VEGF-B, and PlGF.
Visual Outcomes:
- Eylea HD has similar visual acuity improvements as regular Eylea but with the advantage of fewer injections due to its longer-lasting formulation. Its visual benefits are comparable to Eylea, as it targets VEGF-A, VEGF-B, and PlGF.
Anatomical Outcomes:
- Eylea HD reduces macular edema and central retinal thickness like the original Eylea, with the potential advantage of requiring fewer injections due to the extended duration of action from its enhanced formulation.
To summarize, Anti-VEGF drugs, including Eylea, Vabysmo, and Avastin, work by blocking the action of VEGF, a protein responsible for abnormal blood vessel growth and fluid leakage in diabetic retinopathy. Eylea HD is a modified version of Eylea that offers the same anti-VEGF benefits but with a longer-lasting formulation, reducing the need for frequent injections. In contrast, steroids (like Ozurdex) reduce inflammation and fluid buildup but can increase the risk of eye pressure and cataracts with long-term use.
It’s important to note that while these treatments can significantly manage and improve the symptoms of diabetic retinopathy, they are not cures. They help control the disease, reduce swelling, stabilize vision, and prevent further damage, but ongoing monitoring and treatment may be necessary to maintain eye health over time.