By: Ayah Samara & Fabiha Karim
Introduction: Presented in this case is a male patient born in 1952 who was initially admitted for a stroke on August 1st. The patient’s new chief complaint upon re-admission was decreased vision in the left eye since August 17th. This report focuses on the ophthalmological evaluation and management of the patient’s left eye vision loss.
Case Presentation: The patient, a 71-year-old male, presented to our facility with a history of stroke on August 1st. He complained of decreased vision in his left eye since August 17th. He was re-admitted to our hospital for further evaluation. Due to the concerning visual symptoms, an ophthalmologist was consulted for a comprehensive eye examination.
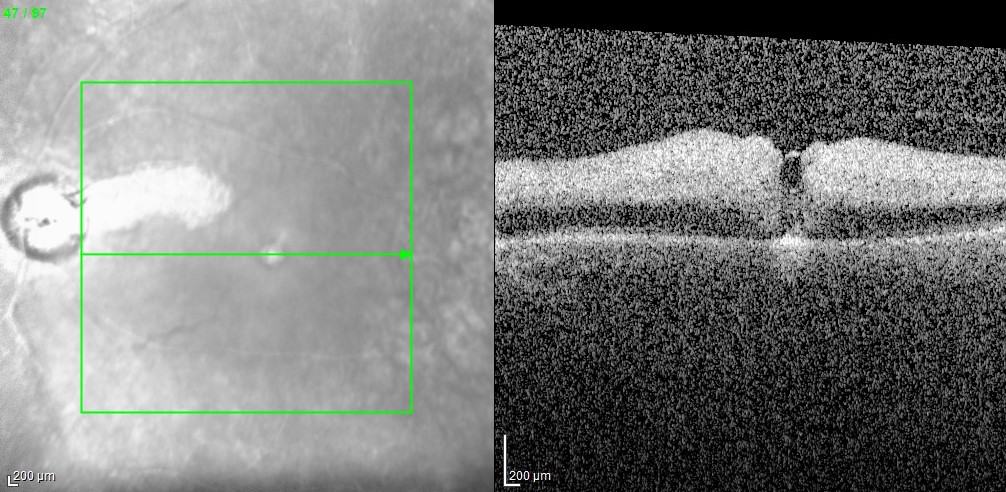
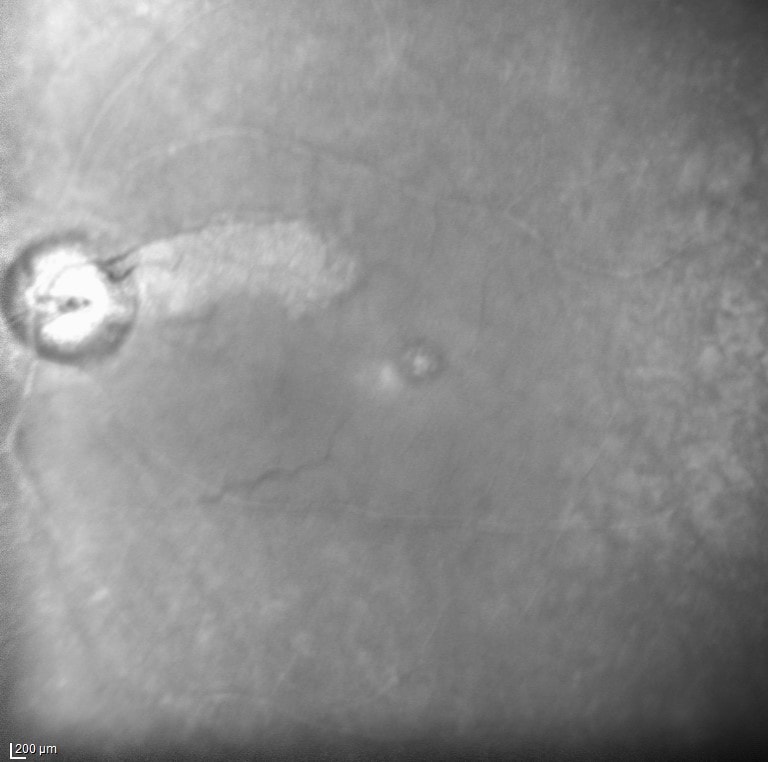
Ophthalmological Examination: Upon examination by our ophthalmologist, Dr. Shah, the patient’s visual acuity in the left eye was found to be reduced to 20/40. Fundoscopic examination revealed a left eye cilioretinal artery perfused with a central retinal artery occlusion. Further scrutiny showed the presence of several cholesterol plaques in the retinal arterioles, suggestive of an embolic event. Optical Coherence Tomography (OCT) scan of the left retina showed inner retinal edema with preservation of the outer retina, particularly in the distribution of the cilioretinal artery. Additionally, infrared imaging demonstrated retinal pigment epithelium preservation corresponding to the distribution of the cilioretinal artery.
Discussion: The patient’s medical history included a previous stroke for which he underwent thrombectomy. Unfortunately, the thrombectomy resulted in a subarachnoid hemorrhage due to reperfusion, rendering double anticoagulation contraindicated. Despite the occurrence of a new embolic event leading to a central retinal artery occlusion, the primary concern remained the patient’s overall life. Therefore, the decision was made to postpone double anticoagulation until the subarachnoid hemorrhage had resolved. The ophthalmologist emphasized that, in such cases, life must take precedence over vision.
Conservative Measures and Management Options: Given the constraints of anticoagulation, the patient’s management included conservative measures to attempt reperfusion of the retina. These measures were tailored to the patient’s unique medical history and risk profile. The rarity of the situation was underscored by the ophthalmologist, who highlighted the fortunate preservation of central vision thanks to the rare presence of the cilioretinal artery, which only 15% of patients have. Normally, vision is decreased to 20/200 or worse in a central retinal artery occlusion without a cilioretinal artery present. The patient’s intraocular pressure will be reduced with topical drops to maintain perfusion to the fovea and remaining retina. The patient will also be monitored for neovascularization of the retina and angle to prevent “90 day glaucoma.”
Conclusion: In conclusion, this case underscores the intricate interplay between ophthalmological concerns and the patient’s overall medical condition. Central retinal artery occlusions can present in the context of complex medical histories, requiring tailored management approaches. The rarity of a perfused cilioretinal artery, which played a critical role in preserving central vision, highlights the importance of early ophthalmological evaluation and collaboration with specialists to optimize patient outcomes.