By: Labh Patel and Shreya Redlam
A 54-year-old female patient visited the clinic for the evaluation of potential macular degeneration with choroidal neovascular membrane in her left eye. The referring physician suggested injecting anti-VEGF into the left eye to treat “wet” macular degeneration. For a few months, the patient had been experiencing intermittent blurry vision in her left eye associated headaches, and floaters. The left eye had a mild afferent pupillary defect and extensive pigmentary atrophy centrally. During the examination, subretinal pigmentary changes and drusen were present in both maculae. Fundus photos are shown below:
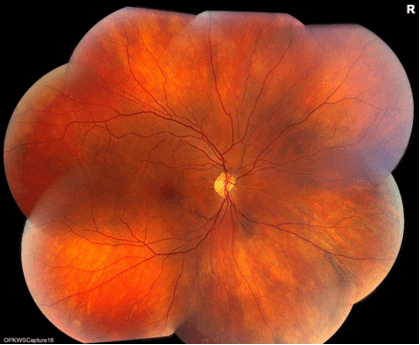
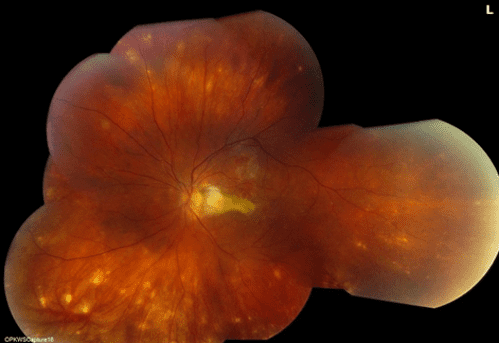
Figure 1: Fundus montages imaging in both eyes. Posterior pigmentary changes are visible in both eyes, with drastically more changes in the left eye. Also, the left eye displays peripheral white-yellow lesions.
To better understand the disease, fluorescein angiogram, fundus autofluorescence, and indocyanine green angiography were performed. These were done with regards to the left eye’s asymmetry and peripheral lesions.
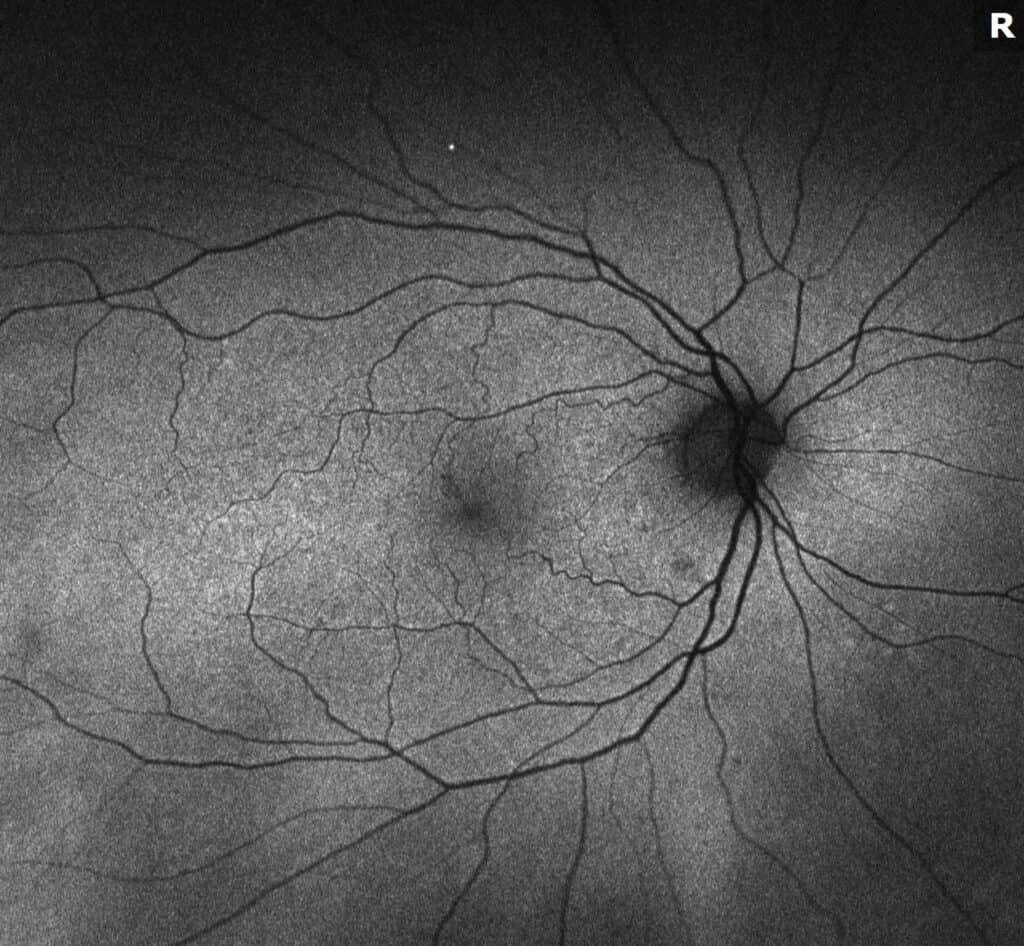
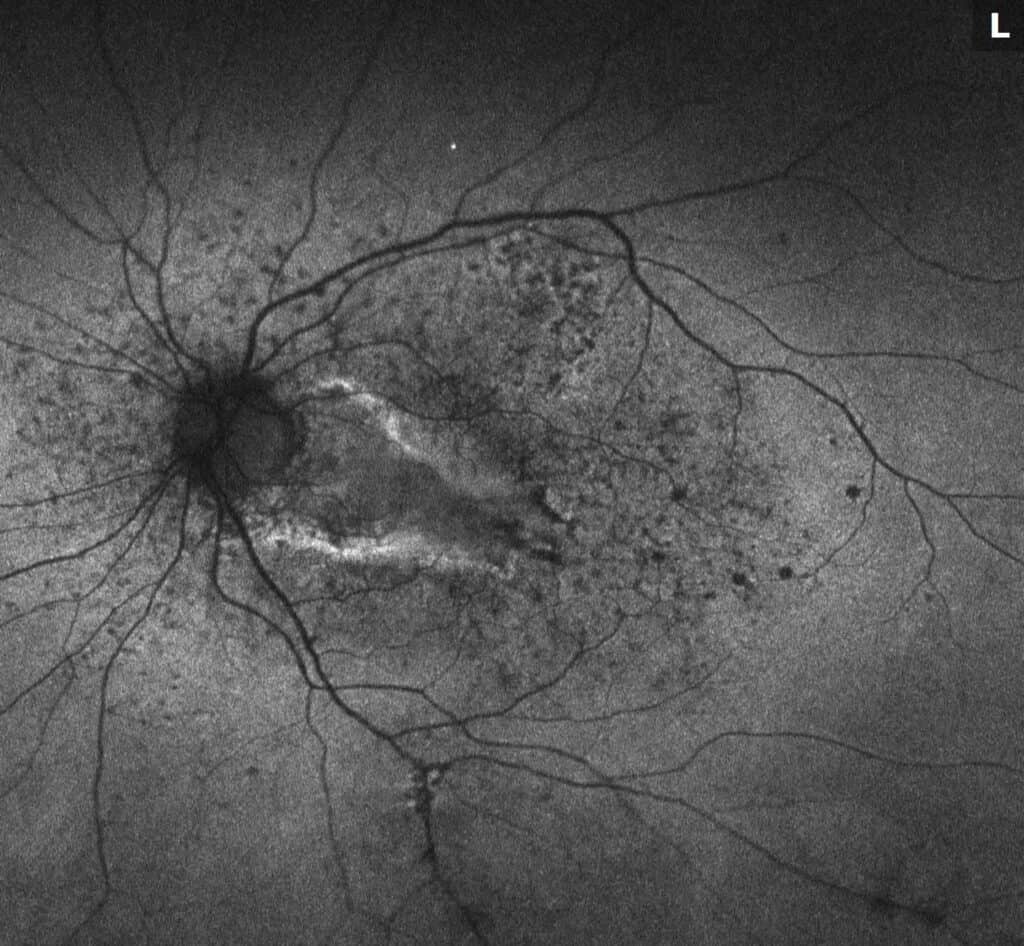
Figure 2: Fundus autofluorescence images. The right eye displays normal autofluorescence consistent with drusen. The left eye shows mixed hyper- and hypo-autofluorescence, which are seen with both subretinal fibrosis and drusen.

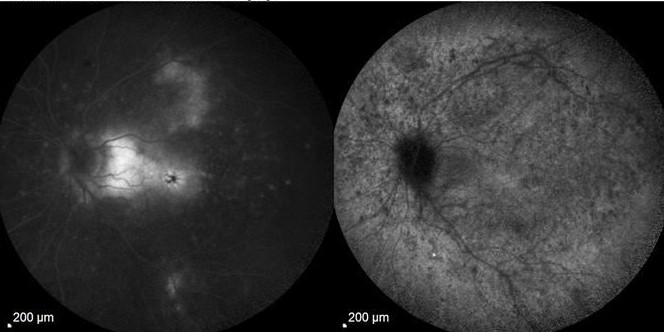
Figure 3: Fluorescein angiogram (FA) with indocyanine green angiography (ICG) images. The right eye displays late staining of drusen, which is visible on FA. There is a hypocyanescence inferonasal to the nerve which is seen with a choroidal lesion of unknown significance on ICG. Early staining of subretinal fibrosis and late leakage of cystoid macular edema are visible.
Additional history was obtained from the patient about peripheral lesions, asymmetry of disease, and extensive scarring of the left eye in a pattern that is not normal for AMD. One year ago, the patient reported sudden loss of vision and was referred to a neuro-ophthalmologist with the possibility of optic neuritis or ischemic optic neuropathy. She was treated with IV Solumedrol for 3 days with improvement but then did not make it to a follow-up appointment and realized drastic vision loss. The retinal lesions were taken note of during her next visit to her comprehensive ophthalmologist, who then referred her to our office.
The afferent pupillary defect indicated a history of optic nerve inflammation. The differential diagnosis was broadened from the referral for choroidal neovascular membrane related to macular degeneration due to the white dots in the periphery and subretinal fibrosis. Additional lab testing aided in narrowing down to non-infectious entities. Oral steroids, the typical treatment in MFCPU, were begun. In order to diminish her cystoid macular edema, local anti-inflammatory and anti-VEGF injections were used. The cystoid macular edema improved after this. Unfortunately, the subretinal fibrosis in the macula slowly stopped progressing. The patient was given steroid sparing immunosuppressive therapy (methotrexate) in response, and she is doing well.
MFCPU is an idiopathic, inflammatory disease that results in bilateral inflammation in an episodic pattern. Patients with this disease typically have multiple chorioretinal lesions (unseen in our patient). The white dots in this disease are much bigger than those that are visible in punctate inner choroidopathy (PIC). In opposition to presumed ocular histoplasmosis syndrome (POHS), vitritis is common. Treatment can help avoid full vision loss. The general eye professionals were right in seeing and identifying drusen in her eyes, but the patient also had a more subtle, uveitic reason for her left retinal fluid, which could have been treated earlier at our clinic to prevent additional fibrosis/scarring. Early referral to a retina specialist is vital, as seen in this case.
References
1. Essex, Rohan W., et al. “Idiopathic Multifocal Choroiditis.” Retina, vol. 33, no. 1, 2013, pp. 1–4., doi:10.1097/iae.0b013e3182641860.
2. Goldstein, Debra, and Lary Ulanski. “Multifocal Choroiditis vs. PIC: Variations on a Theme?” Review of Ophtalmology, 2004.
3. Pinar, Vakur, and Stephen Foster. “Bilateral Chorioretinal Lesions Appearing Late in Posterior Uveitis.” 2000.
4. Dolz-Marco, Rosa, et al. “How to Differentiate Myopic Choroidal Neovascularization, Idiopathic Multifocal Choroiditis, and Punctate Inner Choroidopathy Using Clinical and Multimodal Imaging Findings.” Ophthalmic Surgery, Lasers and Imaging Retina, SLACK Incorporated, 16 Mar. 2017,
5. Li, J., Li, Y., Li, H. et al. Imageology features of different types of multifocal choroiditis. BMC Ophthalmol 19, 39 (2019). https://doi-org.ezproxy.med.ucf.edu/10.1186/s12886-019-1045-x